Rowan's Law

Concussion Awareness Resource
Preventing injuries is important to keeping people active throughout their lives. Some injuries are easy to see and treat but what about an injury inside the head? Brain injuries, such as concussions, don’t show on the outside and are not always obvious. Even when you can’t see the injury, a person with a concussion still feels the effects and needs the proper care to get better.
This resource will help you learn more about concussions so you can keep yourself and others active and safe – whether you’re an athlete, student, parent, coach, official or educator.
What is a concussion?
A concussion is a brain injury. It can’t be seen on X-rays, CT scans or MRIs. It may affect the way a person thinks, feels and acts. A concussion is a serious injury. While the effects are typically short-term, a concussion can lead to long-lasting symptoms and even long-term effects, such as memory problems or depression.
What causes a concussion?
Any blow to the head, face or neck may cause a concussion. A concussion may also be caused by a blow to the body if the force of the blow causes the brain to move around inside the skull. Examples include being hit in the head with a ball or falling hard onto the floor.
When can they happen?
Concussions can happen in any sport and are more likely to happen when the athlete does not expect the force or impact. Concussions are difficult to assess and manage because the symptoms can begin shortly after the injury or take a longer time to appear. You may experience a variety of symptoms. In adults, most of the concussion symptoms resolve within 10 to 14 days.
How is a concussion assessed?
It is critical to stop playing your sport immediately after having a suspected concussion. A sport-related concussion/mTBI can be recognized within the community by athletes, parents, coacher, officials, trainers, and licensed healthcare providers. Formal diagnosis should be made by a healthcare provider, following a thorough medical assessment. You will be looked at for signs of concussion as well as severe head, neck, or spine injury. You will also be monitored for a few hours after having a suspected concussion.
Do not return to the game or practice until a primary healthcare provider approves your return. Accurate diagnosis, management, and return to sport decisions are important at all levels of sport and for all types of sport.
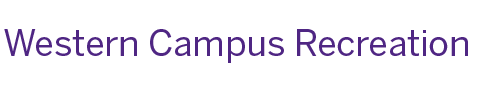
Recognizing a concussion

Everyone can help recognize a possible concussion if they know what to look and listen for.
A person with a concussion might have one or more of the signs or symptoms listed below. They might show up right away or hours, even days, later. Just one sign or symptom is enough to suspect a concussion. Most people with a concussion do not lose consciousness.
Common signs and symptoms of a concussion:
PHYSICAL:
- Headache
- Pressure in the head
- Dizziness
- Nausea or vomiting
- Blurred vision
- Sensitivity to light or sound
- Ringing in the ears
- Balance problems
- Tired or low energy
- Drowsiness
- “Don’t feel right”
EMOTIONAL:
- Irritability (easily upset or angered)
- Depression
-Sadness
-Nervous or anxious
COGNITIVE (THINKING):
- Not thinking clearly
- Slower thinking
- Feeling confused
- Problems concentrating
- Problems remembering
SLEEP-RELATED:
- Sleeping more or less than usual
- Having a hard time falling asleep
RED FLAGS:
“Red flags” may mean you have a more serious injury. Treat red flags as an emergency and call 911.
- Neck pain or tenderness
- Double vision
- Weakness or tingling in arms or legs
- Severe or increasing headache
- Seizure or convulsion
- Loss of consciousness (knocked out)
- Vomiting more than once
- Increasingly restless, agitated or aggressive
- Getting more and more confused
What to do if you suspect a concussion
If you suspect a concussion, remove yourself or the person you are supervising from the activity right away. Continuing to participate puts you or the person with a suspected concussion at risk of more severe, longer-lasting symptoms. Call the parent/guardian (for athletes under 18 years of age) or emergency contact. Don’t leave anyone with a suspected concussion alone.
Anyone who has been removed from sport with a suspected concussion should see a physician or nurse practitioner as soon as possible. That person should not return to unrestricted participation in training, practice or competition until they have received medical clearance.
Getting Better
Most people with a concussion get better in one to four weeks. Some people take longer. Each concussion is unique – don’t compare one person’s recovery to another’s.
It’s possible for a concussion to have long-term effects. People may experience symptoms, such as headaches, neck pain or vision problems, that last for months, or even years. Some may have lasting changes in their brain that lead to issues such as memory loss, concentration problems or depression. In rare cases, a person who suffers multiple brain injuries without healing in between may develop dangerous swelling in their brain, a condition known as second impact syndrome, that can result in severe disability or death.
While a person is recovering from a concussion, they shouldn’t do activities that may make their symptoms worse. This may mean limiting activities such as exercising, screen time or schoolwork.
Healing from a concussion is a process that takes patience. Rushing back to activities can make symptoms worse and recovery longer.
Anyone who has a concussion should let others know. This includes parents, all sport teams/ clubs, schools, coaches and educators.
And remember, returning to school comes before returning to unrestricted sport.
Returning to School and Sport
Athletes and students who are diagnosed by a physician or nurse practitioner as having a concussion must proceed through their sport organization’s return-to-sport protocol and/or, where applicable, their school board’s return-to-school plan.
Athletes and students should work with their healthcare professional and sport organization/school to establish their individual plans to return to sport as well as return to school.
The Return-to-School Plan (Learning and Physical Activity)
Students in elementary and secondary school will need to follow their school board’s return- to-school plan, which supports a student’s gradual return to learning and return to physical activity. Contact the school for more information.
The Return-to-Sport Protocol
Most return-to-sport protocols suggest that athletes should rest for 24 to 48 hours before starting any gradual return to sport. An athlete must not resume unrestricted participation in training, practice or competition until they have received medical clearance.
The table below provides a list of steps and activities that are commonly found in most return-to-sport protocols and return-to-school plans.
|
Table: Common Steps in Graduated Return-to-Sport Protocols |
|||
|
Step |
Aim |
Activities |
Goal of Step |
|
1 |
Symptom-limiting activities
|
Daily activities that don’t make symptoms worse, such as moving around the home and simple chores |
Gradual re-introduction of daily school and work activities
|
|
2 |
Light aerobic activity |
Light activities that increase the heart rate just a little, such as walking or a stationary bicycle for |
Increase heart rate |
|
3 |
Sport-specific exercise
|
Individual physical activity such as running or skating No contact or head impact activities |
Add movement |
|
4 |
Non-contact training, practice, drills
|
Harder training drills Add resistance training (if appropriate) |
Exercise, co-ordination and increased thinking
|
|
5 |
Unrestricted practice |
Unrestricted practice - with contact where applicable |
Restore confidence and assess functional skills |
|
6 |
Return to sport |
Unrestricted game play or competition |
|
|
Medical clearance is always required prior to the athlete’s return to unrestricted practice, training or competition. Check with a medical professional for the specific steps that you should follow. |
|||
An athlete is typically ready to progress to the next step when they can do the activities at their current step without new or worsening symptoms. If at any step symptoms get worse, they should stop and go back to the previous step. Each step should take at least 24 hours to complete. If symptoms do not improve or if the symptoms continue to worsen, the athlete should return to the physician or nurse practitioner.
Remember:
- Recognize signs and symptoms of a concussion and remove yourself or the athlete from the sport/physical activity, even if you feel OK or they insist they are OK.
- Get yourself/the athlete checked out by a physician or nurse practitioner.
- Support gradual return to school and sport.
This information is part of a series of Rowan’s Law concussion awareness resources. Rowan’s Law was named for Rowan Stringer, a high school rugby player from Ottawa, who died in the spring of 2013 from a condition known as second impact syndrome (swelling of the brain caused by a subsequent injury that occurred before a previous injury healed). Rowan is believed to have experienced three concussions over six days while playing rugby. She had a concussion but didn’t know her brain needed time to heal. Neither did her parents, teachers or coaches.
These resources are not intended to provide medical advice relating to health care. For advice on health care for concussion symptoms, please consult with a physician or nurse practitioner.
Other Resources:
Rowan’s Law
https://www.ontario.ca/page/rowans-law-concussion-awareness-resources
Concussion Legacy Foundation Canada
https://concussionfoundation.org/concussion-resources
Parachute Canada
https://parachute.ca/en/injury-topic/concussion/
Fowler Kennedy Sports Medicine Clinic
http://www.fowlerkennedy.com/patient-resources/sport-concussion/
Ontario Neurotrauma Foundation
https://braininjuryguidelines.org/concussion/index.php?id=1