DLD Toolbox
Contact Us
Lisa Archibald, PhD
Associate Professor
Western University
School of Communication Sciences and Disorders
Elborn College
1201 Western Rd.
London, Ontario CANADA
N6G 1H1
Tel: 519-661-2111 ext. 82753
Email Dr. Archibald
Follow Dr. Archibald on twitter at @larchiba6!
Identifying DLD in children under 5 years of age
by Lisa Archibald
DLD Diagnostics Flowcharts
- Volume 1: Diagnostic Statements for DLD
- Volume 2: DLD vs. Language Disorder associated with...
- Volume 3: DLD and Test Scores
- Volume 4: Co-occurring or Associated Language Disorder
- Volume 5: Identifying DLD in children under 5-year-old
Scenario: The SLP/SaLT assessment determines that a child under 5 years has language difficulties with a significant impact on everyday interactions & no known biomedical condition. Given the variability in language development at this age, what considerations might help the clinician decide if the problem is likely persistent and a diagnosis of DLD is warranted?
Caveat
Volume 5 of the #DLDToolbox deals with the question of identifying Developmental Language Disorder (DLD) in children under 5 years of age. I found this a challenging volume to create. I relied on evidence examining early predictors (0-4 years) of confirmed DLD, that is, DLD in children 4 years (at minimum) and older. In fact, I gave greater weight to findings from studies examining predictors of DLD in 5 to 11 year old children, which were the oldest children for which I found relevant evidence. Please note that there is much evidence pertaining to outcomes for late talkers, but not all of this evidence was relevant to my focus on DLD (i.e., persistent language disorder beyond preschool). Where relevant, I describe below findings not currently in the volume, but of potential importance with further evidence.
More on the scenario
Please take careful note of the diagnostic scenario for volume 5. The scenario starts after the SLP/SaLT has completed their assessment (including appropriate tests, gathering of information from the family, etc.). At the point the scenario begins, we already know 3 pieces of information about the child: (1) a completed SLP/SaLT assessment has determined the presence of language difficulties, (2) a significant functional impact on everyday social interactions has been confirmed, and (3) there are currently no known biomedical conditions diagnosed.
Let’s compare what we know about this child to the CATALISE definition of DLD:
|
DLD Definition |
Vol. 5 Diagnostic Scenario |
|
Persistent |
|
|
Language difficulties |
√ Language difficulties |
|
With a significant impact on everyday interactions or school learning |
√ Significant impact on everyday social interactions |
|
Not associated with a known differentiating biomedical condition (see vol. 4) |
√ No currently diagnosed biomedical conditions |
As you can see from this table, the remaining question in this scenario is around persistence. Are the observed language difficulties likely to be persistent? The reason this is a tricky question is because we know that language development is variable in children under 5 years old. Population-based studies of late talkers indicate that a considerable portion recover and some children who were not late talkers go on to have language difficulties. We also know that it’s difficult to predict which children will have persistent language difficulties. The Early Language in Victoria Study (https://www.mcri.edu.au/elvs/researchfindings) has lots of information on this topic, and will have lots more to come!
At present, then, there are no language test results (on their own) that can reliably differentiate persistent from transient language difficulties in young children. One easy conclusion to draw from this would be that DLD cannot be identified in under 5-year-olds, BUT, there are lots of reasons for us to find a better answer than this. If we know which children are likely to have persistent language difficulties, we can better focus our intervention and resources on them and we can better empower families to provide the support and advocacy their child will need. This flowchart brings together available evidence to help clinicians determine if a diagnosis of DLD is warranted in children under 5 years.
Orientation to the flowchart
The flowchart summarizes indicators across a number of factors relevant to language outcomes. Indicators on the far left (with a red underlay) would raise low concern because they are associated with positive outcomes. If the majority of a child’s indicators fall in this zone, then a diagnosis of DLD would NOT be given. In this case, we would use the term ‘language difficulties’, and we would continue to monitor the child for continued signs of resolving language issues. The indicators in the middle (with a yellow underlay) would raise moderate concern. None of these, on their own, would be enough to warrant a diagnosis of DLD, but they would indicate a child who needs to be monitored closely and their response to enhancements or interventions assessed. The indicators on the far right (with a green underlay) would raise considerable concern because they are associated with persistent language difficulties. If the majority of a child’s indicators fall in this zone, the diagnosis of DLD is worth strong consideration. Here’s a dilemma, though: a young child with severe language impairment across multiple domains might be highly likely to have a persistent language disorder (as in DLD), but they might also be more likely to have a differentiating biomedical condition (e.g., autism) warranting the diagnosis of ‘Language Disorder associated with {biomedical condition}. In such a case, using the overarching term ‘Language Disorder’ might be sufficient. Please also refer to volume 4 for additional guidance on DLD vs. Language Disorder associated with {biomedical condition}. Across all of these diagnostic decisions, please note that avoiding the term ‘language delay’ is recommended both because we can’t use the term with any precision and because we don’t want to underplay the significance of the observed language difficulties.
Notes on the factors included
I hope that the factors included on the flowchart are fairly self-explanatory, but here are some additional notes on each one:
|
Age |
The older the child is when language difficulties are observed, the more likely those difficulties are to be persistent. Essentially, persistence is very hard to predict in under 2-year-olds. Language difficulty in 4+ year-olds, however, is very likely to be persistent. Three-year-olds are in the middle ground. |
|
Time over which re-assessment has indicated continued language difficulties |
The CATALISE studies suggested re-assessing late talkers after 6 months. You might see a child more frequently, but continued language difficulties after 6 months would be a strong indicator of persistence. Of course, this factor is influenced by the child’s age. If a child has language difficulties over 6 months but they are still only 2.5 years old, it's probably still too early to diagnose DLD. |
|
Language domains impacted |
The listed domains were described in the CATALISE studies. There is no way to quantify ‘few’ vs. ‘many’ domains. The note references Bishop & Edmundson (1987) who found good outcomes for those with isolated impairments and stable profiles of language impairment in those with phonology, morphology, syntax, and semantic impairments. Children with impairments in phonology only (only, only) might be better described as having a speech sound disorder, and their prognosis is favourable. The presence of receptive language deficits, however, suggests a poorer prognosis. |
|
Risk factors |
We need to be cautious when considering risk factors because taken together, they still do not have great predictive power. The presence of multiple risk factors conveys a moderate level of concern, not more. The listed risk factors were identified over multiple studies with consistency, except in one case: The risk factors listed under ‘other’ were reported less consistently or in fewer studies, and were grouped in order not to inflate their weighting. |
|
Early gestures or language indicators |
The listed indicators were reported in a population-based study and over more than one study. There are studies that have reported lower use of communicative gestures and more tantrums in toddlers and preschool children with language difficulties. However, given the lack of studies demonstrating the predictive power of these skills for persistent DLD, they were not included in the flowchart. Clinicians might consider these signs with caution. |
|
Later preschool language indicators |
Later preschool probably equates to 3.5 years and older. The later preschool language indicators came from a study by Bishop and Edmundson, which included participants ages 3.9-4.2 years. |
|
Malleable factors |
Malleable factors are those factors that are expected to change when circumstances are changed. In the case of a child with language difficulties, altering one of these factors will shed light on the persistence of the problem. A positive response to changes in these factors would lend confidence to a decision for the absence of a disorder. A lack of change, or change only with considerable effort, would be more indicative of a persistent problem. When quality input is not available, ongoing concern would be warranted. When discussing enhancements to the child’s language & literacy environment, it is important that families understand that the enhancements are to address the child’s language difficulties and are not reflective of any prior lack in the child’s environment. |
Case examples
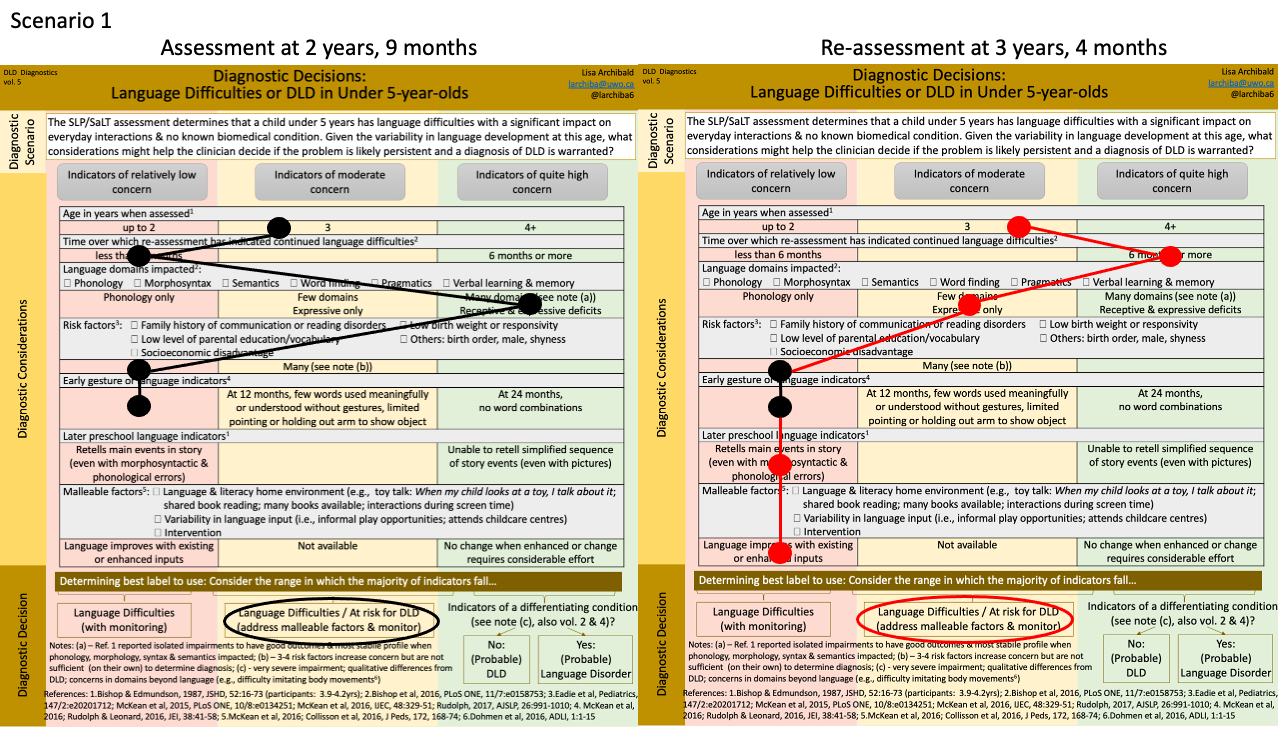
Although I didn’t design the flowchart to be used in this way, I’ve created 2 scenarios with the indicators marked with circles for each child. In Scenario 1, a child is first assessed at 2 years, 9 months of age and again at 3 years, 4 months. At the earlier assessment, difficulties in expressive and receptive language skills were observed, although word combinations were used meaningfully. There were also no significant risk factors. Nevertheless, the mixed expressive-receptive deficits in a child over 2 years of age was of sufficiently high concern to warrant the identification of Language Difficulties with a need to address malleable factors. Parents began using a dialogic reading approach at home, and the child participated in a language-enhancing intervention group. The child was re-assessed 7 months later. Receptive language difficulties were resolved, and the child was able to retell events of a story. The positive response to changes in the malleable factors and resolving language difficulties suggests that the language difficulties might be transient. Nevertheless, the persisting difficulties in a child over 3 years old warrants ongoing concern and the continued identification of language difficulties with a need to address malleable factors. In another 6 months, the continued persistence of Language Difficulties may warrant identification of DLD whereas a continued pattern of resolution would lessen concern.
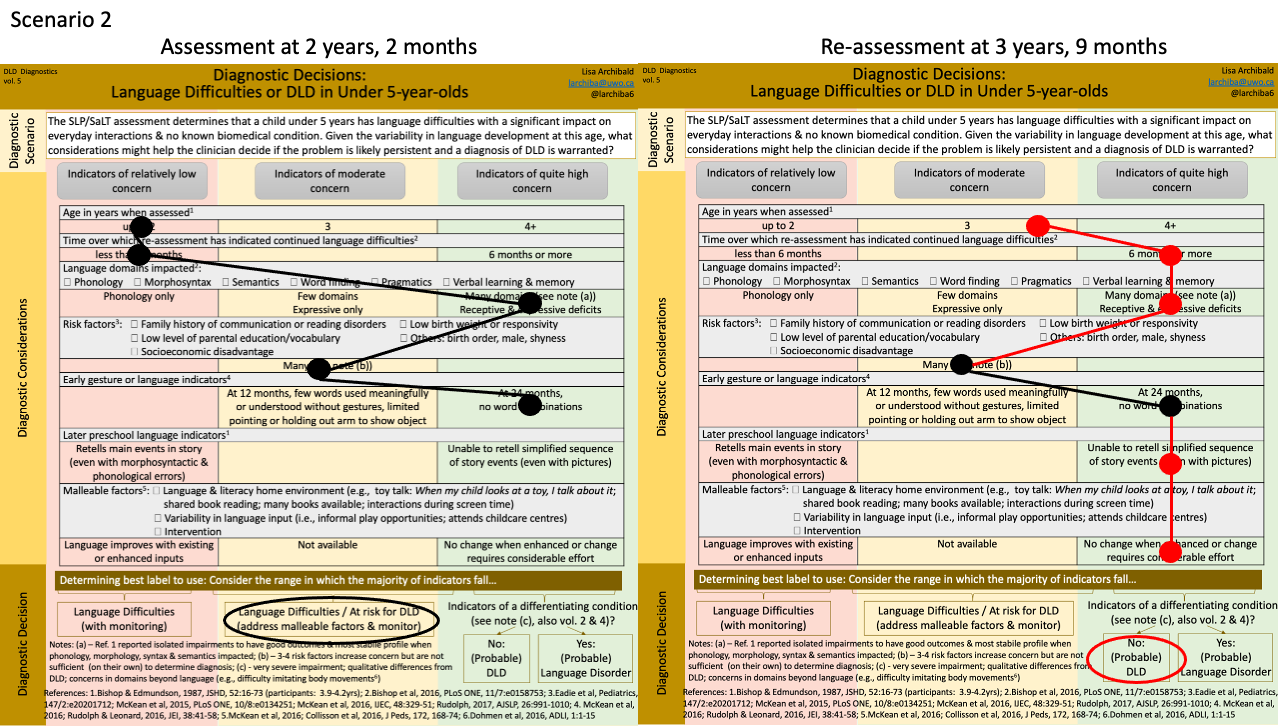
In Scenario 2, a child is first assessed at 2 years, 2 months and again at 3 years, 9 months. (I’m sure there were other services in between!) At the earlier assessment, mixed receptive-expressive deficits and a lack of 2-word combinations along with the presence of many risk factors warrant high concern. The child is identified with Language Difficulties with a need to address malleable factors. A number of language & literacy enrichments are adopted by the family, and intervention is provided. At the later assessment, despite the concerted effort to address malleable factors, the mixed receptive-expressive deficits persist and the child is unable to retell a simplified sequence of story events. Nevertheless, there are no concerns regarding biomedical conditions. A diagnosis of DLD is provided.
Final remarks
Determining the presence of Developmental Language Disorder (DLD) in children under 5 years of age can be challenging. Volume 5 of the #DLDToolbox provides some guidance, but it’s not foolproof. Clinical judgement is required. Thanks for striving to make the best clinical judgement you can, and helping families support children with language difficulties.

